by Paul Ingraham, Vancouver, Canada.
About Paul Ingraham please visit: https://www.painscience.com/about-paul-ingraham.php
Article copied from: https://www.painscience.com/articles/patellofemoral-pain-and-vastus-medialis.php
January, 2017
Can just one quarter of the quadriceps be the key to anterior knee pain?
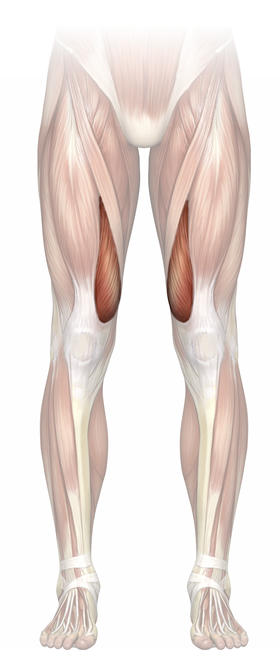 The most knee jerk exercise prescription for patellofemoral syndrome (PFPS) is to strengthen not just the quadriceps but one measly quarter of the quads. Practically everyone who seeks professional care for the condition gets told to specifically train the vastus medialis obliquus (VMO) muscle — the section of the quadriceps that is on the inside of your thigh, which pulls on the inside edge of your kneecap. This is widely regarded as the gold standard of therapy for patellofemoral pain. It needs to be demoted.
The most knee jerk exercise prescription for patellofemoral syndrome (PFPS) is to strengthen not just the quadriceps but one measly quarter of the quads. Practically everyone who seeks professional care for the condition gets told to specifically train the vastus medialis obliquus (VMO) muscle — the section of the quadriceps that is on the inside of your thigh, which pulls on the inside edge of your kneecap. This is widely regarded as the gold standard of therapy for patellofemoral pain. It needs to be demoted.
Quadriceps strengthening is actually an effective treatment,1 just not because of the VMO — but in countless cases the VMO gets the credit when general thigh training is what did the trick. Exasperating!
Meet the quadriceps
The quadriceps muscle is actually four muscles that merge at the kneecap (hence the Latin “quad”). There’s the fairly skinny rectus femoris section on top, and then three big vasti sections on the outside, centre, and inside of the thigh: the vastus lateralis, vastus intermedius, and medialis. The kneecap’s position is partially determined by the “tug-of-war” between these muscles. Alleged tracking problems, with their unknown (but probably trivial) significance, occur in theory because either the vastus lateralis is pulling too strongly, or because the vastus medialis is pulling too weakly, or a bit of both, or due to a problem with the timing (coordination) of contraction — for instance, both sides may be strong enough, but if the contractions aren’t well coordinated the effect may be asymmetrical. And so on.
The clinical significance of tracking has already been debunked earlier in this book. (Eh? What book?2) Quick review: Peeler et al found that there is “no significant correlation between any of VM insertion length, VM fiber angle, limb alignment, and patellofemoral joint dysfunction location and severity [of pain]”3 and Balcarek et al established that the VMO is identical in people with and without unstable patellofemoral joints.4 If the VMO is relevant to the stability of this joint, it involves no visible differences in the muscle. Any atrophy that might have been found could just as easily be attributed to disuse because of pain — not vice versa.
And how about functional differences? Much the same (as beaten to death in the chapter “Weak and uncoordinated muscles, perhaps?”): studies have found no differences in the timing activity of the VM in people with PFPS compared to those without. And again, if there was such a difference, it could be a symptom.
But here’s the punchline, the coup de grace on this topic, the final VMO uh oh…
Is it possible to “isolate” vastus medialis contraction?
None of the above really matters one way or the other if we can’t actually train the VM to pull its weight. To do that, we need a way of making it contract more than the other parts of the quadriceps: “isolation,” or at least emphasis, of VM contraction. But is that possible?
Debunkers like myself have said no, often and loudly, for many years. I’ve called VM isolation a “pernicious myth,” based one evidence like Mirzabeigi et al 5 — one of many studies over the years that strongly suggested VM isolation was either impossible (or only possible in the sense that what you see at Cirque du Soleil is possible, but out of the reach of the average person). In 2002, Malone, Davies, and Walsh wrote, “The concept of VM isolation through specific exercise should no longer be part of our lexicon.”6 Such professional opinions have been common for a decade and they are still out there.
We were wrong-ish.
More recent evidence has mostly changed my mind. At least six recent studies — all admittedly small, but also all quite straightforward and probably adequate — have shown that just the right exercises do indeed preferentially engage the VM. Not dramatically, but a bit. For whatever it’s worth. And, interestingly, the methods were quite diverse…
- squats with some isometric hip adduction (squeezing your knees together)7
- a leg press exercise in the deepest part of the range, plus isometric hip adduction8
- sqatting on very unstable surfaces9
- squatting slowly with biofeedback10
- squats with a wedge (standing on a wedge so that the toes are pointing down)11
- deeper squats12
It’s a little surprising to me that just “deeper squats” does the trick, even a little bit. Did we really have to wait until 2016 for that discovery? Was that really missed by previous investigations? Science is a slow process!
So it’s possible to “isolate” the VM. But of course, none of these studies demonstrated anything like real “isolation” of the VM, just the VM contracting somewhat more relative to the other parts of the quadriceps. Although I should probably never use the word “impossible” again, it’s unlikely that any average person can contract the VM on its own, or even anywhere close to it, under any circumstances. That would be like trying to do a squat using just your butt muscles but no hamstrings — good luck with that.
So what if you can preferentially contract the VM? Does it actually matter?
None of these studies have anything directly to do with the treatment of patellofemoral pain—no one has even attempted to show that selectively strengthening the VM works better than any other kind of training. I’ve already presented a lot of evidence that strongly suggests that weak contraction is probably not the cause, so fixing it probably isn’t the solution. There’s no direct evidence that it doesn’t, but at least one study tried to answer the question indirectly, and found that patellofemoral joint kinematics and contact pressures were not significantly influenced by VM strength.”13
Even if the VM is weak in PFPS patient, it’s not obvious that strengthening it is any kind of magic bullet.14
Given everything else we know, I think it’s likely that any benefits that seem to come from VM training are actually just due to exercising the quadriceps as a whole.
That said, when it’s time to exercise, I don’t see any reason not to emphasize VM contraction on a “just in case” basis. Do some deeper squats and leg presses. Do them while pinching your knees together. Squat on a wobble board. The evidence says you will be activating your VM a little more… for whatever it’s worth. Hooray?
NOTES
- 1. Kooiker L, Van De Port IG, Weir A, Moen MH. Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2014 Jun;44(6):391–B1. PubMed #24766358.
- 2. This article is an excerpt from an e-book about patellofemoral pain syndrome: Save Yourself from Patellofemoral Pain Syndrome! By coincidence, the tracking chapter I just mentioned is also available as an excerpt: see Patellofemoral Tracking Syndrome.
- 3. Peeler J, Anderson JE. Structural parameters of the vastus medialis muscle and its relationship to patellofemoral joint deterioration. Clinical Anatomy. 2007;20:307–314.
- 4. Balcarek P, Oberthür S, Frosch S, Schüttrumpf JP, Stürmer KM. Vastus medialis obliquus muscle morphology in primary and recurrent lateral patellar instability. Biomed Res Int. 2014;2014:326586. PubMed #24868524. PainSci #54036.
- 5. Mirzabeigi E, Jordan C, Gronley JK, Rockowitz NL, Perry J. Isolation of the vastus medialis oblique muscle during exercise. Am J Sports Med. 1999;27(1):50–3. PubMed #9934418.
- 6. Malone T, Davies G, Walsh WM. Muscular control of the patella. Clin Sports Med. 2002 Jul;21(3):349–62. PubMed #12365232.
- 7. Irish SE, Millward AJ, Wride J, Haas BM, Shum GL. The effect of closed-kinetic chain exercises and open-kinetic chain exercise on the muscle activity of vastus medialis oblique and vastus lateralis. J Strength Cond Res. 2010 May;24(5):1256–62. PubMed #20386128.
- 8. Peng HT, Kernozek TW, Song CY. Muscle activation of vastus medialis obliquus and vastus lateralis during a dynamic leg press exercise with and without isometric hip adduction. Phys Ther Sport. 2013 Feb;14(1):44–9. PubMed #23312731.
- 9. Hyong IH, Kang JH. Activities of the Vastus Lateralis and Vastus Medialis Oblique Muscles during Squats on Different Surfaces. J Phys Ther Sci. 2013 Aug;25(8):915–7. PubMed #24259884. PainSci #54116.
- 10. Yoo WG. Effects of the slow speed-targeting squat exercise on the vastus medialis oblique/vastus lateralis muscle ratio. J Phys Ther Sci. 2015 Sep;27(9):2861–2. PubMed #26504311. PainSci #54119.
- 11. Lee TK, Park SM, Yun SB, et al. Analysis of vastus lateralis and vastus medialis oblique muscle activation during squat exercise with and without a variety of tools in normal adults. J Phys Ther Sci. 2016 Mar;28(3):1071–3. PubMed #27134414. PainSci #53705.
- 12. Jaberzadeh S, Yeo D, Zoghi M. The Effect of Altering Knee Position and Squat Depth on VMO : VL EMG Ratio During Squat Exercises. Physiother Res Int. 2016 Sep;21(3):164–73. PubMed #25962352.
- 13. Lee TQ, Sundusky MD, Adeli A, McMahon PJ. Effects of simulated vastus medialis strength variation on patellofemoral joint biomechanics in human cadaver knees. Journal of Rehabilitation Research & Development Vol. 2002 une 2002. PainSci #56868.
- 14. The whole “weak and uncoordinated muscles” idea makes PFPS sound like the awkward teenager of knee problems, which is not true — many elite athletes with strong and coordinated quads get this problem! And making a weak muscle a little stronger won’t necessarily make it more functional. The baseline activity of a muscle is not determined by its maximal strength. Otherwise, bodybuilders’ muscles would be seizing them up and tearing their muscles from their bones. Muscles contract to provide just the right amount of force for a particular task, using both the commands of the brain and the feedback of the senses. How this all works is the endlessly interesting field of study called motor control. But all you need to know is this: just because a car is capable of going fast, doesn’t mean it always goes fast. It just can go faster, if needed. Think of muscles similarly.
Descargar PDF – Articulo – Patellofemoral Pain & the Vastus Medialis Myth








Sigueme en Redes Sociales